You
are working in TCC when EMS arrives, bagging an unresponsive elderly-appearing
female. They report that
they were called to a nursing home for unresponsiveness, and found the patient
on the floor. On their arrival,
she was minimally responsive to noxious stimuli and had a heart rate of 36 on
the monitor. She received atropine
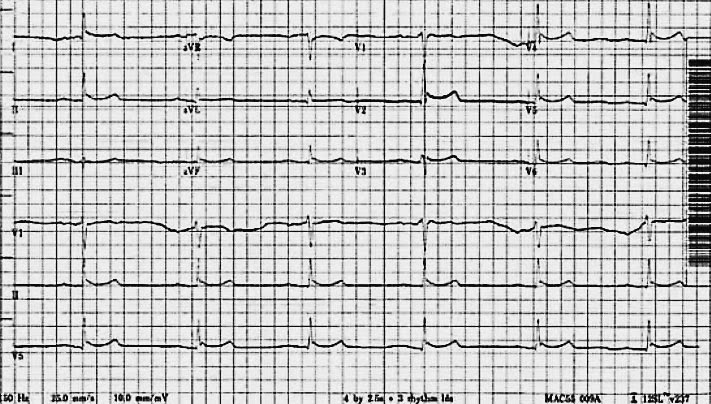
0.5 mg x 3 prehospital with minimal response. Her blood pressure is 80/60. To identify if there is heart block, you get an EKG
demonstrating marked sinus bradycardia with a 1st degree AV block
and possible ST elevation in the inferior and precordial leads (see below):
You
intubate the patient, and as you are placing pacer pads on, your attending
notes that she feels very cold to touch.
Her temperature by Foley catheter?
28.2 degrees! You take
another look at the EKG and think – ah, not ST elevation after all, but J
waves.
After
initating the patient on some aggressive rewarming with warmed IV fluids, a
bear hugger and warmed ventilator circuit, you take a moment to ask two
questions:
[1] Above and beyond the J
waves of Osborn, what EKG findings are suggestive of/associated with
hypothermia?
Luckily
for you, emergency medicine EKG guru Amal Mattu wrote a paper on this very
subject. Entitled simply, “Electrocardiographic
Manifestations of Hypothermia” it goes through a series of cases and highlights
a few important take homes regarding EKGs in hypothermic patients:
a. The
J-wave is the most common EKG finding in hypothermia, and is found when core body
temperatures are < 32 ˚C. They
can be seen in other situations as well, including subarachnoid hemorrhage,
acute cardiac ischemia, and normal normothermic patients.
b. Atrial and ventricular arrythmmias become more
predominant with the degree of hypothermia. Marked sinus
bradycardia with decreased AV conduction velocity (as seen in this patient)
is a common finding.
c.
Intervals (as in all of them) can be prolonged.
d. A
pseudoinfarction, with ST elevation, pattern is sometimes seen. The pattern should resolve with
re-warming.
e. The EKG will not necessarily reflect the peaked T
waves of hyperkalemia. Be wary,
this subset of “found down” patients can have hyperkalemia secondary to rhabdo
or renal failure, but it won’t be as noticeable in the EKG.
Importantly,
the intervention for the above arrythmmias is not anti-arrythmmics , pacing, or
even pressors as these have limited utility in a cold myocardium. The treatment is re-warming (see below), which will resolve most of the above.
[2] What is the differential diagnosis for
hypothermia – i.e., what tests should I send and what interventions should
happen for this critically ill patient in the emergency department?
Remember,
once you diagnose the patient with hypothermia, your workup and interventions do
not stop there – hypothermia has a differential diagnosis: (see ref 2)
A. Horses – environmental
exposure, severe
hypothyroidism, diabetic ketoacidosis, sepsis,
multisystem trauma, and prolonged cardiac arrest
B. Zebras – Hypothalamic lesions, episodic hypothermia with
hyperhydrosis
Therefore, there are two main components of
the ED intervention:
1. Diagnose and treat the underlying cause – Check TSH, Initiate septic workup and broad spectrum antibiotics.
2. Aggressive rewarming –There are four classifications for types of rewarming
a Passive external – i.e. blankets – raises temp 0.5 – 4˚C/hr
b. Active external – i.e BEAR hugger – raises temp 1-2˚C/hr
c. Active internal – humidified vent, warm IV fluids, body cavity lavage - raises temp 0.5 – 1.2˚C/hr
d. Extracorporal – ICY lines and ECMO – raises temp 4-10˚C/hr.1. Diagnose and treat the underlying cause – Check TSH, Initiate septic workup and broad spectrum antibiotics.
2. Aggressive rewarming –There are four classifications for types of rewarming
a Passive external – i.e. blankets – raises temp 0.5 – 4˚C/hr
b. Active external – i.e BEAR hugger – raises temp 1-2˚C/hr
c. Active internal – humidified vent, warm IV fluids, body cavity lavage - raises temp 0.5 – 1.2˚C/hr
a, b, and c are usually sufficient for mild to moderate hypothermia.
In
the ER, the patient was intubated, aggressively warmed with a humidified vent,
warm IV fluids and a bear hugger - and had a concordant rise in her heart rate and blood
pressure and resolution of her EKG findings:

Clinical takehome – Be suspicious of
hypothermia in patients with cardiogenic shock who are found down. Remember, a
lot of your “go to” interventions will not work in these patients. Treat hypothermia and related cardiac
complications with aggressive rewarming, and don’t forget that hypothermia has
a differential diagnosis.
References:
[1]
Mattu, A., Brady, W. J., & Perron, A. D. (2002). Electrocardiographic
manifestations of hypothermia. The
American journal of emergency medicine, 20(4),
314-326.
[2]
Aslam, A. F., Aslam, A.
K., Vasavada, B. C., & Khan, I. A. (2006). Hypothermia: evaluation,
electrocardiographic manifestations, and management. The American journal of medicine, 119(4), 297-301.
Interested
in some more learning about J waves?
AliEM
on J waves: http://lifeinthefastlane.com/ecg-library/basics/osborn-wave-j-wave/
and remember to look out for EKG challenge #2 next week.
Contributed by Maia Dorsett, PGY-3
No comments:
Post a Comment