As we discussed on our last Paper Trail post, the results of the ARISE and ProCESS trials seem to indicate that the most meaningful interventions for a patient in severe sepsis/septic shock are early antibiotics & source control and aggressive resuscitation in an appropriately-monitored environment.
At our shop, we're currently working on analyzing our own sepsis response data and designing new protocols. In these discussions, some have expressed concern over the potential for giving too much fluid to these patients. The concepts of "fluid responsiveness" and "fluid tolerance" are the subject of much debate in the FOAMed critical care world these days.
(See the discussions between Drs. Marik and Weingart over at EMCrit for reference.)
Our own ED Critical Care guru, Dr. Christopher Holthaus, stepped up to the plate and offered his views on fluid resuscitation of septic patients in the ED:
"The fluid issue can be challenging. Although some studies suggest that an early restrictive fluid strategy potentially may bear a signal [toward improved outcomes], the preponderance of current ED-based RCTs involving patients with severe sepsis and septic shock will have up-front ED volumes of 4-6L and are showing the best mortalities to date (approx. 18%). [See comparative table below delineating up front/early fluid volumes PROCESS vs ARISE -- Ed.]
"Although any patient is at risk for volume overload during a resuscitation, patients in these studies appear to have tolerated these volumes relatively well with low adverse events as far as acute pulmonary edema (< 0.02%). We know patients do worse if they are dry and get placed on pressors. Somewhere in between probably lies the truth. Perhaps better exact timing of fluid administration when the heart is truly volume-responsive (i.e., on the ascending portion of the Starling curve) will be the way to go. It remains to be seen, but this approach hypothetically may also show the same overall total volume in the end...
"Nevertheless, perhaps in the meantime a more judicious rule of thumb is to discriminate "early vs. late" in the resuscitation, and to acknowledge that patients with distributive shock from sepsis generally have trouble maintaining intravascular volume and/or blood pressure during SIRS-related events. Unfortunately we don’t have any great immediate fixes for that yet besides giving volume (or pressors), treating the source, and supportive care.
"Providers dealing with these patients early in their presentation (i.e., first 6-8 hours) are supported in administering total fluid volumes of 4-6 L (Rivers’ EGDT, PROCESS, ARISE). The RCT using an ED early restrictive fluid strategy for these patients does not exist yet. In current practice, most providers will bolus the first 1-2 L on presentation and perhaps another 500-1000 mL "PRN" based on various factors -- fluid tolerance, tachycardia, hypotension, urine output. The argument for a maintenance rate in these patients is supported by Figure S2 from the PROCESS trial [shown below - Ed.] which used maintenance rates of 250-500 mL/hr once a SBP > 100 or Shock Index < 0.8 were achieved with boluses. This point alone was perhaps one of the best contributions from PROCESS in regards to demonstrating a proven objective alternate fluid administration strategy which went beyond the original use of CVP for quantitative resuscitations.
"Because the ED currently does not have a go-to gold standard outcome study for gauging volume responsiveness via dynamic changes in stroke volume in these patients, we are left with the fluid volume quantity and rates which stands as the current best available evidence (i.e., 4-6 L in first 6-8 hrs parsed between boluses and maintenance rates).
"In the end, of course one size does not fit all and clinical judgment individualized to the patient is always warranted."
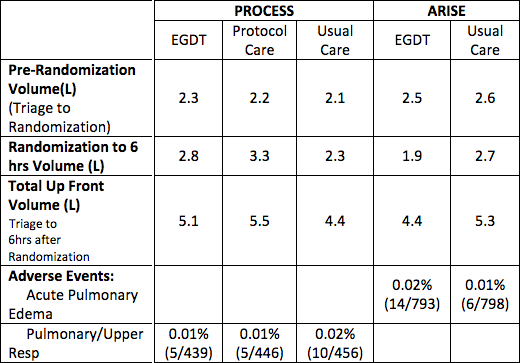 |
| Adopted from ARISE & ProCESS data by Holthaus CV. |
 |
| Protocol for Standard Therapy arm of ProCESS trial (Supplmental Figure S2) |
What do you think? Is fluid overload from ED resuscitation in the "early" phase of sepsis a legitimate concern? When do you pull the trigger and start pressors? Let us know what you think!
Submitted by Christopher V. Holthaus MD.
Copy editing C. Sam Smith, PGY-3.
Copy editing C. Sam Smith, PGY-3.
No comments:
Post a Comment